The Frequently Asked Questions (FAQs) page answers questions providers ask about the BabyNet program and the integration of the BabyNet Reporting & Intervention Data Gathering Electronic System (BRIDGES) and Medicaid Management Information System (MMIS).
Providers should subscribe to receive communications and updates from the South Carolina Department of Health and Human Services (SCDHHS) about the BabyNet program and BRIDGES. "BabyNet" should be selected as a topic of interest.
- Service Coordination and Special Instruction/Family Training FAQs
- Service Provider Claims and Payments FAQs
If a BabyNet child has private insurance and Medicaid/Part C, what information do I enter into the Accounts Payable Screen in BRIDGES?
If the provider accepted the third-party payment amount as payment in full, Medicaid cannot contribute to the claims payment. If a BabyNet beneficiary has private insurance, TPL is applicable to the claim.
Providers MUST wait to receive their EOBs from the third-party payors before submitting claims.
After providers receive their EOBs from third-party payors, they can enter information into the accounts payable screen.
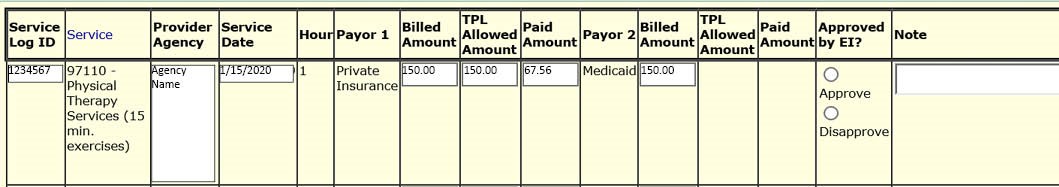
In this scenario, for Payor 1, the provider billed $150.00. The private insurance allowed amount (on the EOB) is $150.00 and the private insurance actually paid $67.56. In Payor 2, the provider should enter in the billed amount for this claim – not what providers are “billing” Medicaid/Part-C; the Billed Amount for Payor 1 and Payor 2 is the same - $150.00. Then the provider can save and submit this claim.
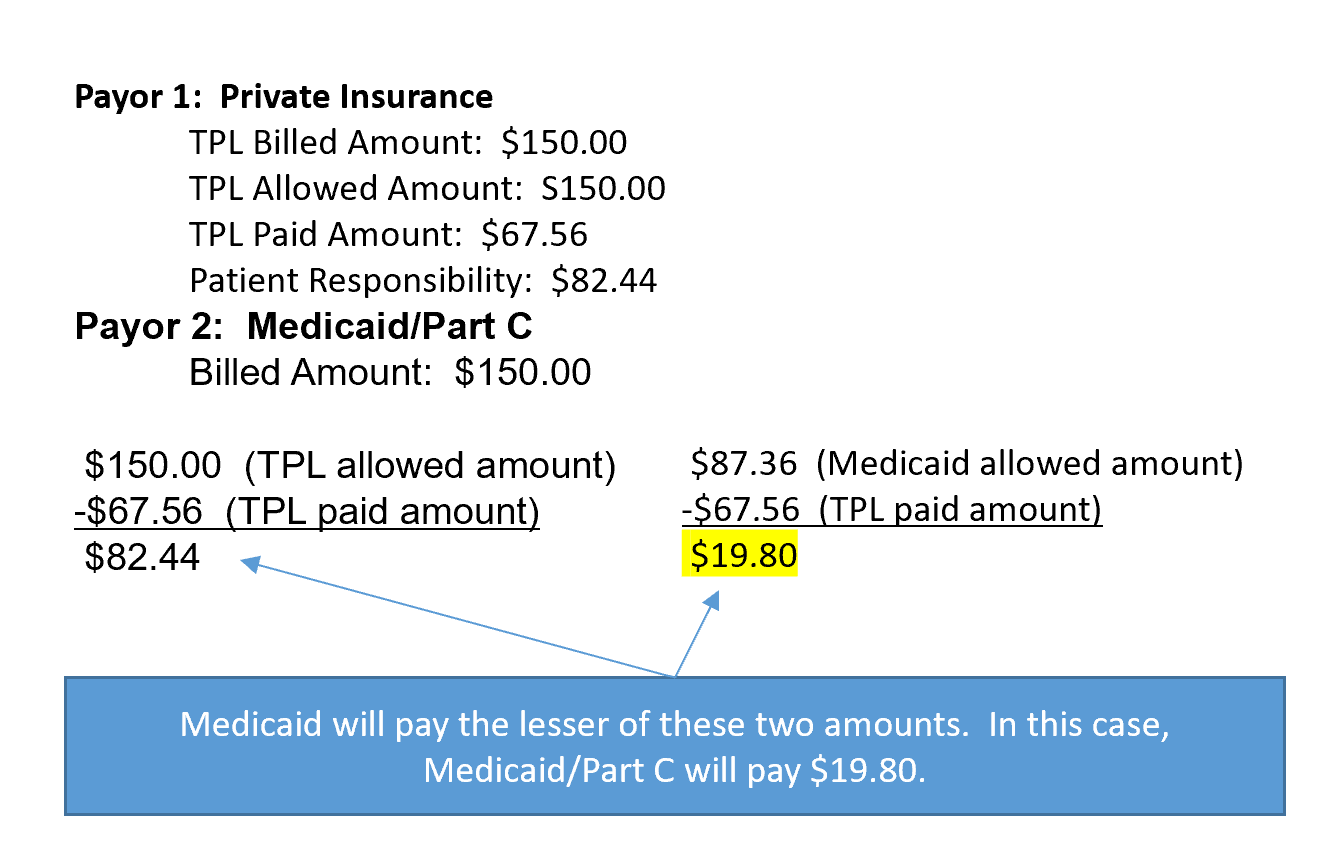
In this example, this claim would be submitted through BRIDGES and then transmitted to MMIS where TPL logic would be applied. The Medicaid Allowed Amount for 97110 is $21.84/unit, and in this case, there were 4 units of 15 minutes, or an hour. The total Medicaid Allowed Amount for this scenario is $87.36.
The provider billed for $150.00 for the hour, and private insurance paid $67.56. The provider then entered the billed amount ($150.00) for the hour and saved and submitted the claim.
The Patient Responsibility in this scenario is $82.44 ($150.00 - $67.56). Medicaid will pay the lesser of the Patient Responsibility and Medicaid allowed amount minus other insurance payment.
In this scenario, the Medicaid allowed amount minus the other insurance payment is $19.80.
Medicaid will pay $19.80 since it is less than the patient responsibility of $82.44. See below.
Providers need to use the remittance advice available in the SCDHHS web tool to manage their accounts receivable/balance their books, and not base it on the information that is available in BRIDGES.
Read more information about TPL. View the Medicaid fee schedules.
How to update TPL information if a patient gains or loses a third-party payor?
It is the service coordinator's responsibility to maintain current TPL information for all children and to submit that to SCDHHS as a child’s TPL information changes. To do so, service coordinators must completely fill out the Health Insurance Information Referral Form (HIIRF). View instructions on how to complete and submit the HIIRF.
If a provider is aware of a gain/loss of a child’s third-party payor, they must notify their service coordinators of this change.
How does a provider enroll with Medicaid/Part C?
BabyNet providers must enroll with both the Medicaid and BabyNet programs, and their two respective systems – MMIS and BRIDGES. Providers should follow both programs’ unique processes on how to enroll.
Please remember that information submitted to both programs must be consistent, i.e. enrolling the correct and same NPI and taxonomies in both systems. Inconsistent data entered into the two systems may result in mismatched information, which may lead to claims being denied.
View more information on how to enroll with BabyNet. View more information on how to enroll with Medicaid.
Please remember, assistants cannot enroll with Medicaid. To meet MMIS requirements, assistants must use the NPI of their supervisor who is enrolled in BRIDGES.
How can I avoid payor source errors in BRIDGES?
During the integration of BabyNet with Healthy Connections Medicaid, the planned services screen must be set up correctly in BRIDGES to avoid payor source errors for children’s coverage.
View a Billing Companion Guide for BRIDGES.
Providers: Do NOT enter a Service Log if a payor source is missing or out of order.
How can I reconcile BabyNet claims payments for claims with dates of service on and after Nov. 1, 2019?
Providers will access their remittance advice in the SCDHHS web tool for dates of service after Nov. 1. View an example of the Claims Submission, Processing and Payment Cycle.
Providers can reference their remittance advice to respectively identify the BabyNet and Medicaid claims payment amounts that they receive from the South Carolina Treasurer’s Office.
Should I bill the SCDHHS web tool directly for BabyNet claims?
No. Providers must bill through BRIDGES.
Providers should enter service logs and billing information through BRIDGES for dates of service that occurred on or after July 1, 2019. Entering billing information in both BRIDGES and the SCDHHS web tool may result in the claim rejecting or the provider receiving an overpayment payment, which will require SCDHHS to take action to recoup payment for any services that were double billed.
All providers, including those serving children enrolled in Medicaid Managed Care Organizations (MCO), must continue to enter service logs into BRIDGES to ensure complete data collection, program oversight, and federal reporting. Providers must bill respective MCOs directly when rendering services to a BabyNet member who is in an MCO.
If a child has private insurance and FFS Medicaid, will BabyNet pay if the private insurance and FFS Medicaid do not pay the full amount for dates of service after Oct. 1?
No. With the integration of BabyNet and Medicaid, BabyNet rates are now aligned with Medicaid’s. As previously announced, SCDHHS will no longer accept balance billing. Medicaid systems will now adjudicate BabyNet claims and payments.
Medicaid computes an allowable amount for a procedure. If payments received by other insurance companies are equal to or greater than the Medicaid allowed amount, Medicaid will not make a payment.
When other payments received are equal or greater than the Medicaid allowed amount, any Medicaid or BabyNet copayment must be refunded to the beneficiary. Medicaid will not make a payment greater than the amount that the provider has agreed to accept as payment in full from a third-party payor.
If the other insurance payment is less than the Medicaid allowed amount, Medicaid will contribute the lesser of either the Medicaid allowed amount minus the other insurance payment, or the sum of the provider plan’s patient responsibility. The patient’s responsibility is their copay, coinsurance and deductible that is normally contributed by the patient outside the insurer’s contribution to the claim. Medicaid reimbursement is considered payment in full.
For example, if a provider did not receive a Third-Party Liability (TPL) payment amount as payment in full for a service they rendered and the Medicaid allowed amount for this service is $200, but the TPL pays $130 for the procedure and the patient’s responsibility for the procedure is $25, Medicaid will contribute the patient responsibility amount because it is less than the difference between the Medicaid allowed amount minus the TPL payment. The TPL Calculator can further depict various scenarios.
It is providers’ responsibility to check eligibility for additional insurance besides Medicaid and BabyNet. Providers can check eligibility in the SCDHHS web tool and by contacting their service coordinators.
Read more information about TPL.
The order of payors is as follows:
- Child has private insurance and Medicaid: no Part C funds are used, private insurance is billed first and Medicaid pays last
- Child has private insurance only: private insurance is billed first and the remainder of their allowed balance may be paid by Part C
- Child has no public or private benefit: Part C pays for services
- Managed Care Organization (MCO) FAQs
In order to receive payment through an MCO for services during the continuity of care period, BabyNet providers must submit to the MCO:
- The Universal BabyNet Prior Authorization form
- A copy of the IFSP (the print screen on planned services screen); and,
- A complete and accurate claim form to the appropriate MCO.
- If providers have questions for a specific MCO, they should contact them directly. View MCO contact information.
Service coordinators must identify BabyNet beneficiaries who are enrolled in an MCO and receiving services from a non-credentialed provider.
In addition, during the continuity of care period, providers may not accept new MCO-enrolled beneficiaries unless the provider is also credentialed with the MCO in which a beneficiary is enrolled.
BabyNet providers MUST be an enrolled Medicaid provider prior to seeking enrollment and/or credentialing by an MCO.
Credentialing and contracting with an MCO is required in order to be eligible for payment by an MCO. The credentialing process requires a completed credentialing application for each MCO you intend to bill for Medicaid BabyNet services. The credentialing process can take up to 60 days after the proper submission of an accurate and complete application. SCDHHS has provided a listing of BabyNet providers that are enrolled in Medicaid to the MCOs for the purpose of reviewing the composition of their current networks with respect to BabyNet providers.
If a BabyNet child loses Medicaid eligibility (FFS or MCO), do providers have a way to bill BabyNet for services rendered to that BabyNet child?
Providers need to routinely check Medicaid eligibility for members in the SCDHHS web tool. If the eligibility status in the SCDHHS web tool does not match what is in BRIDGES, providers and/or service coordinators should contact BabyNet@scdhhs.gov to request that the eligibility information be updated. Providers should be able to bill accordingly once this information is updated in BRIDGES.
Any services on the IFSP must be provided at no cost to the family. Providers cannot stop rendering services to BabyNet children based their eligibility status in BRIDGES.
Because Medicaid and Part C are the same payor on planned services, these services should be paid with no changes made in BRIDGES. Planned services only need to be updated if third-party liability is lost or gained.
Do parents have to provide consent to allow BabyNet to bill their Medicaid and/or private insurance?
Because the Part C lead agency is also the Medicaid agency, the U.S. Department of Education, Office of Special Education Programs (OSEP) has clarified that permission is not required for billing Medicaid or private insurance for children who are Medicaid eligible.
If a child has private insurance and is in an MCO, will BabyNet pay if the private insurance and the MCO do not pay the full amount?
Medicaid reimbursement will be made for covered services up to the lesser of the provider-billed amount or the Medicaid allowed amount. In cases where a primary insurer has made a payment, the Medicaid allowed amount shall be reduced by any primary payer reimbursement amount. Medicaid reimbursement is considered payment in full.
The order of payors is as follows:
- Child has private insurance and Medicaid: no Part C funds are used, private insurance is billed first and Medicaid pays last
- Child has private insurance only: private insurance is billed first and the remainder of their allowed balance may be paid by Part C
- Child has no public or private benefit: Part C pays for services
Will Part C pay for services if a child loses Medicaid?
Part C is always the payor of last resort. If a child loses Medicaid or private insurance, Part C will pay for services.
Will BabyNet/Part C pay for services denied by an MCO?
No. MCOs are responsible for claims administration for their enrolled members.
Do therapy assistants have to be credentialed with the MCOs?
No, only therapists.
If we find that a child has two Medicaid numbers, which Medicaid number should be used for billing?
Please email BabyNet@scdhhs.gov.
Will providers need to monitor the number of allowed units for BabyNet eligible children who are enrolled with an MCO?
It is recommended that providers monitor the number of billed units for all BabyNet children. Providers are required to submit the IFSP to the MCOs as prior authorization for payment up to the number of approved units on that document. Billing for units above the approved number on the IFSP will result in a denial of payment.
Are children able to receive (therapy) services via BabyNet and from a freestanding (non-BabyNet) provider at the same time?
BabyNet members are eligible to receive services up to the approved units on the IFSP, which will serve as the prior authorization for services. The prior authorization is specific to the service provider listed on the IFSP. Any additional services may be billed subject to an approved prior authorization specific to the billing provider.
Will MCOs require medical necessity for BabyNet eligible children?
BabyNet providers are required to submit the IFSP to the appropriate MCO in order to be eligible for payment up to the number of approved units on that document. The IFSP will serve as the medical necessity documentation.
Are providers required to enter service noted in BRIDGES for children being served by an MCO?
Yes. Providers will risk not being reimbursed if they do not enter service notes in BRIDGES.
Which MCO's have quality incentive programs and how do you qualify?
Each Healthy Connections Medicaid MCO has a quality incentive program. Providers are encouraged to contact individual MCOs to inquire about program details. Providers can also contact SCDHHS Provider Relations for additional information.
Do we still bill claims in BRIDGES if patient has an MCO?
Providers must enter service logs (or service notes) into BRIDGES for every encounter with a BabyNet eligible child. A claim will automatically be created and transmitted to the Medicaid system once the service log is entered. No additional claims input is necessary in BRIDGES.
If we are already credentialed/enrolled with a specific MCO, does the MCO Universal Prior Authorization Form for BabyNet have to be sent for a patient who is enrolled with that specific MCO, even though a provider is in network with that MCO and has a prior authorization on file with them?
As a rule, providers should follow the guidelines set by each specific MCO governing prior authorizations. During the continuity of care period, the information listed on the IFSP Planned Services page dictates what services and amounts of service are covered. Any services or amounts above what is listed on the IFSP will require prior authorization in order for the claim to be reimbursed.
Prior authorization guidelines in place with MCOs may differ after the end of the continuity of care period. Providers should inquire as to the appropriate process for prior authorizations with their contracting MCO.
About the Universal Prior Authorization Form for BabyNet, do we have to send this in for future authorizations, or can we just get an authorization from the MCO per their requirements?
As a rule, providers should follow the guidelines set by each specific MCO governing prior authorizations. During the continuity of care period, the information listed on the IFSP Planned Services page dictates what services and amounts of service are covered. Any services or amounts above what is listed on the IFSP will require prior authorization to be reimbursed.
I noticed that one child's IFSP end dates changed and was shortened. Will that change our MCO authorization time period that was approved based on longer end date?"
This question should be posed to the relevant MCO for their input. Deviations from the IFSP may require additional authorization.
Will BabyNet pay for the treatments if the MCO denies authorization or service?
The information listed on the IFSP Planned Services page dictates what services and amounts of service are covered. MCOs should pay for services and amounts listed on the IFSP during the continuity of care period. Any services or amounts above what is listed on the IFSP will require prior authorization from the MCO to be reimbursed.
Molina requires an authorization for reevaluations. Often times, providers and EIs are unaware that children have received initial evaluations until the claim has been denied. In order to receive reimbursement, the provider would have to contact the EI and request to have the plan changed to a reevaluation & rebill the service as a re-evaluation, however Molina does not provide retro authorizations. If the resubmitted claim is denied due to lack of authorization, will BabyNet provide the reimbursement?
As a general rule, providers will need to work with individual MCOs to be reimbursed for services provided to BabyNet children enrolled in that MCO. SCDHHS/BabyNet will not pay reimbursements above and beyond what the MCO has agreed to pay a provider in their contract with that provider.
Providers should ensure that all services to be performed are listed on the IFSP correctly before the service is rendered. Claims need to reflect the services listed on the IFSP. Any necessary updates or corrections to the IFSP should be completed by the service coordinator before claims are submitted for payment. Decisions regarding reimbursements for services not listed on the prior authorization are up to each MCO and should be discussed with them.
Because therapy providers have to wait on the EI to enter the therapy onto the BRIDGES planned services page before we can fax the universal authorization request to the MCO, will the MCO be required to backdate the authorizations to match the dates on the Babynet Planned Services Page? OR do providers need to put the child's therapy on HOLD until that info has been entered into BRIDGES and FAXED?
Services listed on the IFSP Planned Services page should not be delayed. Providers should begin to render the services listed on the IFSP and file a claim once the prior authorization paperwork is complete. MCOs should reimburse for services and amounts listed on the IFSP.
I have tried repeatedly to access MCO's reimbursement rates for speech therapy. I do not find it in their manuals. Please help me understand where to find this information or provide current reimbursement rates for the individual MCO's for all therapy services.
Please contact the appropriate MCO for guidance on how to locate this information. A table of contact information has been made available on the SCDHHS BabyNet FAQ page. Providers can also contact SCDHHS Provider Relations at BabyNet@scdhhs.gov for assistance with specific inquiries if there are persistent issues.
I’m looking for clarity regarding if BabyNet providers will have to be contracted with the major insurance companies or just with the Medicaid MCOs?
SCDHHS has requested that BabyNet providers contact the MCOs serving the South Carolina Healthy Connections Medicaid program so that they can become credentialed and contracted. No guidance has been provided regarding contracts with specific insurance companies outside of the Healthy Connections MCOs. SCDHHS does not require contracts with any entity outside of the Healthy Connections Medicaid program.
With these new referrals. Are we able to pick them up if an MCO has all of our paperwork and we are waiting for them to do credentialing?
Providers must be credentialed and contracted with a BabyNet child’s MCO in order to provide services. It can take up to 60 days for MCOs to complete the credentialing process with providers.
How will we know if a child has private insurance, Medicaid (Fee for Service), or Medicaid (Managed Care)?
Private insurance information can be found on the Financial Supports screen. This information will automatically be updated from the Medicaid data system. If a child is Medicaid eligible, the "yes" radio button will be selected at the bottom of the Financial Supports screen and the eligible period will be listed. If a child is in an MCO, the "yes" radio button will be selected at the bottom of the Financial Supports screen and the eligible period will be listed. You will also see the MCO Number (Plan ID) to the right of the radio buttons. This number indicates the child's MCO.
MCO Plan IDs:
- HM1000-First Choice by Select Health of SC
- HM2200-Absolute Total Care
- HM3200-Healthy Blue by Blue Choice of SC
- HM3600-Molina Healthcare of SC
- HM4200-Humana
In the future, how will service coordinators know if a child's payor sources change?
SCDHHS will provide payor source change reports to BabyNet for children with Medicaid. For Part C only children, service coordinators are responsible for getting this information from families (specifically, when a child gains or loses private insurance).
How will we know if a parent gave permission to bill private insurance?
This information should be documented on the Consent to Use Insurance Resources form and should match what it recorded in BRIDGES in the planned services section.
If the child does not have Medicaid, why do they have an SCDHHS number that looks like a Medicaid number?
Because all new referrals are added to Curam, the Medicaid eligibility system, and transferred to BRIDGES, all children will have this number generated. If a child only has BabyNet (Part C), then that number is just referred to as the SCDHHS number. If the child has Medicaid (FFS or MCO), the SCDHHS number is also their Medicaid ID number.
