Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) - Orthodontic Services
The South Carolina Department of Health and Human Services (SCDHHS) will transition the administration of the Early and Periodic Screening, Diagnostic, and Treatment (EPSDT) orthodontic services to its dental administrative services organization (DASO), DentaQuest, effective March 1, 2022. The transition will streamline administrative and payment processes by allowing dental providers to file prior authorization requests and claims to DentaQuest while receiving payment directly from SCDHHS.
There will be a transition period from Jan. 1, 2022, until the effective date of March 1, 2022. During the transition period, providers rendering orthodontic services to South Carolina Healthy Connections Medicaid members under the South Carolina Department of Health and Environmental Control’s (DHEC) Children and Youth with Special Health Care Needs (CYSHCN) orthodontia program must complete the following steps:
1. Enroll in the South Carolina Healthy Connections Medicaid program. Providers can find information and resources on the provider enrollment process at https://www.scdhhs.gov/provider. Providers may use SCDHHS’ online application tool to expedite the enrollment process. For questions regarding enrollment or status of applications, providers should contact the SCDHHS Provider Service Center at (888) 289-0709 or submit an electronic request. A provider enrollment core checklist is detailed in the Orthodontic Services Transition Board available here. In addition, a recorded provider enrollment training is available on SCDHHS’ webpage dedicated to the transition.
2. Once enrollment is completed and the provider is validated in the SCDHHS system, providers must contact the DentaQuest provider representative, Marva Davis, at (803) 250-9340 or marva.davis@greatdentalplans.com, to start the registration process for their DentaQuest account. Dental providers may choose to submit their claims or prior authorizations to DentaQuest in paper format or electronically via web portal, clearinghouse, or HIPAA-compliant 837D file. Information for requirements on each platform is detailed in the Orthodontic Services Transition Board.
3. SCDHHS and DentaQuest will conduct a provider training on Feb. 9, 2022, at 12 p.m., addressing prior authorization and claims filing processes and platforms, policy and benefit limitations and provider web portal features. Providers may participate in the training via:
- Computer or mobile app: Click here to join the meeting
- Call in (audio only): (399) 666-3919; Conference ID: 427 074 306
Login information for the training is also detailed in the Orthodontic Services Transition Board. Providers may also request a personal, in-person or virtual office training by contacting the DentaQuest provider representative, Marva Davis, at (803) 250-9340 or marva.davis@greatdentalplans.com.
4. To allow transferring of all open/active orthodontic cases to DentaQuest, claims or invoices for dates of service up to Dec. 31, 2021, must be filed to DHEC no later than Jan. 10, 2022. All claims for open/active cases with dates of service on or after Jan. 1, 2022, may be filed to DentaQuest beginning March 1, 2022.
Submission of prior authorizations for new cases during the transition period, between Jan. 1, 2022, and Feb. 28, 2022, should continue to be filed with DHEC. Beginning March 1, 2022, all prior authorizations and claims for new and open/active cases must be filed with DentaQuest.
5. Providers must familiarize themselves with Healthy Connections Medicaid policies and procedures, specifically for dental services, available in the Dental Services Provider Manual. Additionally, providers must familiarize themselves with the orthodontic services policy and benefit limitations prior to filing prior authorization requests or claims to DentaQuest. A summary of the Orthodontic Services Policy is available here. The Orthodontic Services Policy will be incorporated in SCDHHS’ Dental Services Provider Manual no later than March 1, 2022. The Handicapping Labio-Lingual Deviation (HLD) Assessment Form is available here.
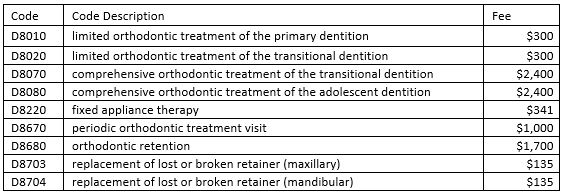
6. Reimbursement for orthodontic treatment will be on per case basis. Reimbursement for each case shall not exceed the Medicaid allowed amount per case, which is $6,100 for comprehensive and $3,000 for limited cases respectively. Payment for each case will be distributed via several installments as described in the Orthodontic Services Policy by billing the following procedure codes appropriate for each case:
For assistance with enrollment or to inquire about application status, providers should contact the SCDHHS Provider Service Center at (888) 289-0709 or submit an electronic request.
For assistance with claims or the prior authorizations submission process through one of the DentaQuest allowed platforms, please contact the DentaQuest Provider Service Center at (888) 307- 6553 or carolinaproviders@dentaquest.com. The three documents and forms mentioned above are also available on the CYSHCN transition page on SCDHHS’ website.